Obstructive sleep apnea is a debilitating condition causing severe pauses in breathing during sleep by partially or completely blocking the upper airways. Both partial and complete forms of apnea impact the sleeper’s oxygen intake, which in turn leads to a range of serious side symptoms and complications. There are three types of sleep apnea—obstructive, central, and mixed apnea. Today we will focus on the most widespread type—obstructive sleep apnea, or OSA. This article will discuss the risk of sleep apnea when a present genetic pattern is determined, the genetic impact on sleep apnea symptoms displayed by a subject in a risk group and how the disorder affect heart disease, hypertension and other most common side effects of OSA.
risk of sleep apnea increase the risk symptoms of sleep apnea heart disease sleep apnea include View first 3
See detailed analysis
Ask any OSA sufferer about sleep apnea symptoms and they will produce a list of these, including interrupted sleep and frequent awakenings to severe daytime sleepiness or fatigue, and, of course, the usual suspect—loud snoring interrupted by gasping sounds. Beneath the tip of the iceberg of OSA signs is an underlying bulk of health complications that the sleeper might not even suspect they are exposed to.
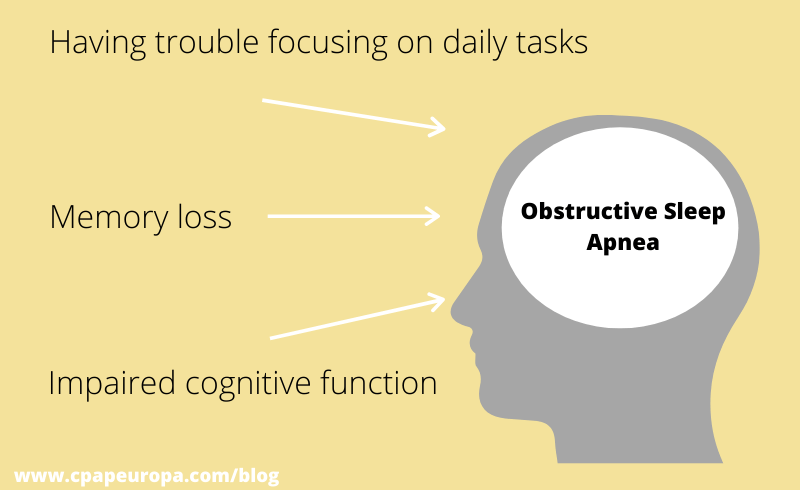
Among these health complications are low blood oxygen levels (hypoxemia), high blood pressure (hypertension), insulin resistance, Alzheimer’s disease and more. The disorder leads to a higher risk of stroke and heart failure, impairs your memory and ability to focus, causes morning headaches, sexual dysfunction and depression. All of the above are caused by what may seem like a simple upper-airway blockage happening at night.
Related articles:
What is sleep apnea and how is it treated?
Catch up on the latest CPAP devices for Positive Airway Pressure therapy
Sleep apnea: frequently asked questions with answers
Does sleep apnea run in the family?
The short answer to this question is: Yes, obstructive sleep apnea is partly hereditary and may run in the family. But this is the overly simplified answer. Unfortunately, nothing about sleep apnea is simple.
OSA is a condition that may be inheritable from first degree family members. For example, children can inherit from their parents their facial features, anatomical characteristics of the upper airway muscles, high body-mass index and tongue size. The anatomy of the tongue may be passed through in family history and lead to developing OSA as the tongue affects the apneic collapse of the soft tissues in the upper-airway during sleep.
The longer answer to this important query, however, needs to be grounded on scientific examination and genetics studies providing concrete results. This is what this article will explain today—the scientific approach to examining the correlation between OSA and genetics, and how exactly that relates to the broader field of study on sleep disorders up until 2020.
Inheritance across age groups and populations
Sleep disorders are present in all age groups and populations, with a strong evidence of genetic inheritance in disorders like narcolepsy and restless leg syndrome. In the case of obstructive sleep apnea the inheritance pattern is still to be defined. And while the genetic etiology of sleep apnea remains rather unclear, sustainable progress in regard to establishing a relationship between apnea and our genes has been made in recent years, with plenty of scientific data to back that up.
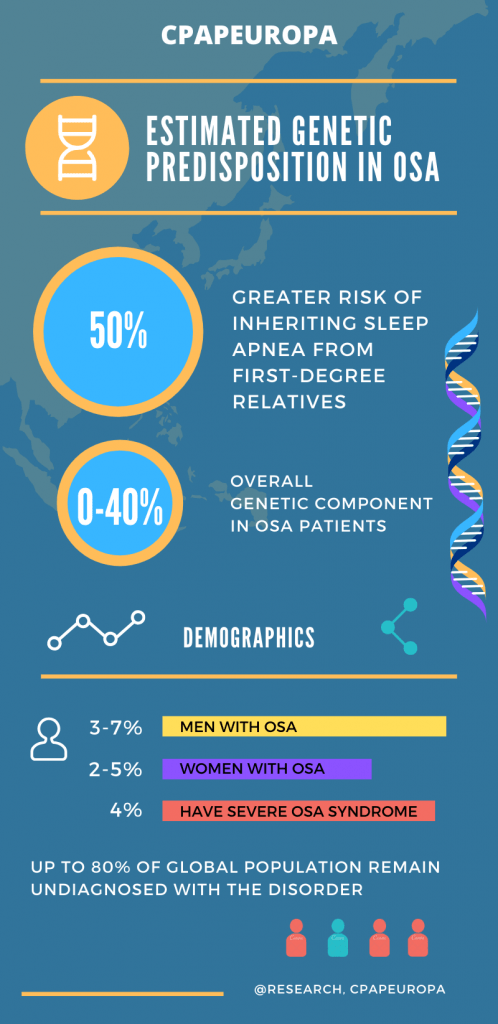
We have already exhausted the topic of risk factors in OSA cases, such as middle age, obesity and gender. The approach to establishing heterogneity and etiology in regards to OSA rests on scientific evidence acquired from documented studies with thousands of volunteering participants across all ages and gender, many of which suggest that the genetic component of OSA in the range of anything between 0 and 40%, while the rest remains in the graph secondary factors.
Inheritance pattern in first-degree relatives
The genetic predisposition in developing sleep apnea still remains largely undefined, in spite of the thousands of conducted studies during the last three decades. Today the inheritance patterns in obstructive sleep apnea (OSA) point to a relation between first-degree relatives with OSA and the presence of the disorder in siblings and children, where the risk of developing apnea is around 50% and greater.
As multifunctional sleep disorder OSA does have a heritable dimension researched primarily through field synopsis and genetic association examination of focus groups of participants. Conducting genetic association OSA studies aims at identifying odds ratios while exploring the connection between population-based and family-based testing. The results try to find an inheritance pattern of OSA by utilizing the existent findings in the developing field of OSA genetics through complex genotyping methods and broad genetic testing.
Genetic sleep apnea testing
Genetic sleep apnea testing analyzes alterations in chromosomes, genes, or proteins in OSA sufferers in order to confirm or exclude a genetic predisposition to the disorder. This type of testing examines the possibility that the patient developed OSA partly due to genetic passing. The methodology utilized in genetic testing is based on gene, chromosomal and biochemical gene tests.
- Gene tests examine the possible variations and mutations in the lengths of DNA that could cause the disorder;
- Chromosomal tests examine long lengths of DNA or chromosomes in an effort to detect major genetic alterations that could lead to the disorder;
- Biochemical gene tests, examine how proteins behave and if they could change the DNA and lead to OSA.
Genetics of neck circumference and OSA explained
The relationship between neck circumference, general obesity and OSA is one of the most well-documented ones to this date. Nine in ten sleep apnea tests asks the same question: ‘Is your neck circumference greater than 17 inches (men) / 16 inches (women)’?
Obesity index, soft palatal length and palate-to-spine angle are constantly studied through research to drive a meaningful correlation between these factors and obstructive sleep apnea. Studies have found that the link between anatomical features and OSA is not as important a factor as neck circumference.
The OSA inheritance factor in obese children
The genetic predisposition and general cause for developing obstructive sleep apnea in children relies on a variety of different factors–both anatomic and neuromuscular. Susceptibility to obstructive sleep apnea in children has proven extremely difficult and is still reliant on future studies and technological advancement. So far studies have shown that children can inherit their parent’s facial anatomy, such as large tonsils and large overbite and chin, which are factors for developing OSA.
Understanding the genetic risk factors as the first step to OSA prevention
In order to encourage early diagnosis and prevention, predictive models in genetic and phenotypic studies need to be established beyond the only suggestive framework of the current results. Steps in OSA prevention can help reduce morbidity and hesitance in the public’s approach to obstructive sleep apnea early diagnosis and treatment by educating the most genetically exposed groups of the population about the risks. The ultimate goal is to reach a proven prescriptive framework that would steer prevention and underline the benefits of early lifestyle changes reducing the chance of developing the disorder in the first place.
Why is it so difficult to understand if OSA is inherited or not?
Just like any other field of study focused on underpinning sleep disorders, genetics research of OSA is focused on early recognition and meaningful results that would increase public awareness about apnea. Until this happens, the genetic foundation of obstructive sleep apnea (OSA) still needs to be established. The difficulty in effectively studying if OSA is hereditary comes from the fact that, so far, physiological metrics across a sufficient range of genetic and phenotypic markers and participants is too costly and invasive to acquire.
The problem with the majority of genome-wide association studies trying to touch upon this extremely challenging topic is that they still remain suggestive instead of conclusive, and that most of them have not been consistently replicated.
The future of OSA genetics studies
Even with large numbers of patients taking participation in OSA studies, coverage across a wide gene region is problematic in regards to obtaining a solid statistical framework in regards to sleep apnea and its genetics origins—especially results that are robust to alternative genetic models. Genetic studies in OSA up to 2020 only find a small non-overlapping relation, without covering enough gene variants to identify a more solid ground for a positive association between the human gene and OSA. Such associations are still subject to variables posing a significant challenge to the global concern that is OSA.
Continue reading Is Sleep Apnea Hereditary: The Genetic Pattern in OSA
 4.8 out of 5 based on 182 reviews
4.8 out of 5 based on 182 reviews