How can you purchase a CPAP device in France?
There are many CPAP (Continuous Positive Airway Pressure) shops in France where you can purchase a CPAP machine from, including CPAP Europa. CPAP is a common treatment for people who have sleep apnea, a sleep disorder in which a person’s breathing is repeatedly interrupted during sleep.
CPAP machines and supplies can typically be purchased at medical supply stores, pharmacies, and online retailers in France. Many of these stores will have trained staff who can assist with fitting and adjusting CPAP masks, as well as answer any questions you may have about using the equipment.
It’s worth noting that some people may be eligible for reimbursement from the French national health insurance system (Sécurité Sociale) for part of the cost of their CPAP equipment, depending on the severity of their condition and the type of treatment prescribed. It is best to check with your doctor and your insurance provider for more information about reimbursement in your case.
If you need to purchase a CPAP machine with express delivery to France, our CPAP shop France is the right place.

Achetez des appareils CPAP ici>>>
Where can you purchase a CPAP device in France?
There are a few different places where you can purchase a CPAP device in France. Some options include:
Medical supply stores: These stores typically carry a wide range of medical equipment, including CPAP machines and supplies. They often have trained staff who can assist with fitting and adjusting CPAP masks and answer any questions you may have about using the equipment.
Pharmacies: Some pharmacies in France also carry CPAP machines and supplies. While the selection may be more limited than at a medical supply store, a pharmacist may still be able to help you with fitting and adjusting a CPAP mask and other basic questions about the device.
Online retailers: There are a number of online retailers in France that sell CPAP machines and supplies, which could be more convenient if you live in a remote area. But it may be harder to get assistance and support with fitting and adjustment of the device and other question, you can reach out to the company’s customer service for support.
Hospitals: Some hospitals also have a medical equipment section where you can purchase a CPAP device, but this is not very common and the selection might be limited.
It’s worth noting that CPAP device and its accessories like masks, tubing, filters and so on are considered as medical device and it requires prescription from a doctor. You should have a prescription from your doctor in order to purchase a CPAP device.
It’s also worth checking with your national health insurance provider to see if they will reimburse you for some or all of the cost of your CPAP device and its accessories, depending on the severity of your condition.


How much does a CPAP device cost in France?
The cost of a CPAP device in France can vary depending on the brand, model, and features of the machine, as well as the retailer or supplier you purchase it from.
On average, a basic CPAP machine can cost between 800 and 1300 euros, while more advanced machines with additional features, such as a built-in humidifier or wireless connectivity, can cost 1500 to 2000 euros. This price is just for the device, accessories like mask, tubing, filters, etc needs to be purchased separately which could cost extra.
It’s worth noting that some people may be eligible for reimbursement from the French national health insurance system (Sécurité Sociale) for part of the cost of their CPAP equipment, depending on the severity of their condition and the type of treatment prescribed. The reimbursement rate is not fixed, it varies from case to case and it is best to check with your doctor and your insurance provider for more information about reimbursement in your case.
It is a good idea to shop around and compare prices from different retailers, both in-store and online, to find the best deal on a CPAP device. Additionally, looking for refurbished or used devices in France can also be a way to save some cost.


How many types of CPAP machines are available for purchase in France?
There are several different types of CPAP (Continuous Positive Airway Pressure) machines available, and the type that is best for you will depend on your specific needs and preferences. Some of the main types of French CPAP machines include:
Standard CPAP: This is the most basic type of CPAP machine in France, and it delivers a constant flow of air at a single pressure setting. This type of machine is best for people who have been diagnosed with mild to moderate sleep apnea.
Auto-CPAP (APAP): This type of machine automatically adjusts the air pressure as needed throughout the night, based on the user’s breathing patterns. Auto-CPAP can be especially helpful for people in France who have been diagnosed with complex or variable sleep apnea.
Bi-Level CPAP (BPAP) : This machine delivers two different pressure settings, one for inhaling and another for exhaling. This is often used for people who has central sleep apnea, where the brain does not send the correct signals to the breathing muscles or for people who have trouble exhaling against a fixed pressure.
Adaptive Servo Ventilation (ASV) : This is the most advanced type of CPAP machine and is used to treat central sleep apnea, which is a form of sleep apnea that is caused by a failure of the brain to send the proper signals to the breathing muscles. This type of machine delivers more precise pressure adjustments to mimic normal breathing patterns and support the user’s natural ventilation.
It’s important to note that CPAP machines are prescribed by doctors and health care provider in France, they will recommend the appropriate machine based on the individual’s sleep study results and medical history.


Is there a difference between CPAP machines currently available in France?
Yes, there are differences between CPAP (continuous positive airway pressure) machines available in France . Some of the main differences include the type of device (fixed pressure vs. auto-adjusting pressure), the size and noise level of the machine, and the presence of additional features such as heated humidifiers and integrated oxygen concentrators.
A fixed pressure CPAP machine delivers a constant, preset level of air pressure throughout the night, while an auto-adjusting CPAP machine, also called APAP, automatically adjusts the pressure as needed to maintain an open airway. Auto-adjusting machines may be more comfortable for some people, but they are generally more expensive than fixed pressure machines.
The size of the machine can also vary, with some models being quite small and portable, while others are larger and designed for home use. The noise level of the machine is another important consideration, especially for people who are sensitive to noise or have partners who are light sleepers. Some machines are very quiet, while others can be quite loud.
Additional features, such as heated humidifiers and integrated oxygen concentrators, can also be important for some people. A heated humidifier adds moisture to the air to help reduce dryness and irritation of the nose and throat. An integrated oxygen concentrator allows the device to deliver both CPAP therapy and oxygen therapy at the same time.
It’s important to note that not every machine is suitable for everyone, different machine are tailored to different specific conditions, it’s important to consult with a healthcare provider to determine the best machine for you.


Is CPAP oxygen or just air?
CPAP (Continuous Positive Airway Pressure) delivers air to the patient’s airway to keep it open during sleep. The air that is delivered through a CPAP machine is typically room air, which is made up of mostly nitrogen (about 78%) and oxygen (about 21%). The air pressure is set to a level that is high enough to prevent the airway from collapsing, but not so high that it causes discomfort.
While CPAP primarily uses room air, some machines can also be equipped with an oxygen concentrator which allows the machine to supply a higher concentration of oxygen, this is called bilevel or BiPAP. However, this use of oxygen through a CPAP device is typically done under physician supervision, mainly used in cases of severe lung diseases, like COPD or heart failure, where a higher oxygen concentration is necessary.
It’s important to note that CPAP is different from oxygen therapy which is delivered through an oxygen concentrator or other device that is specifically designed to provide oxygen at higher flow rates, typically to people with lung conditions such as chronic obstructive pulmonary disease (COPD) or severe cases of sleep apnea where oxygen saturation is low.


What is Obstructive Sleep Apnea?
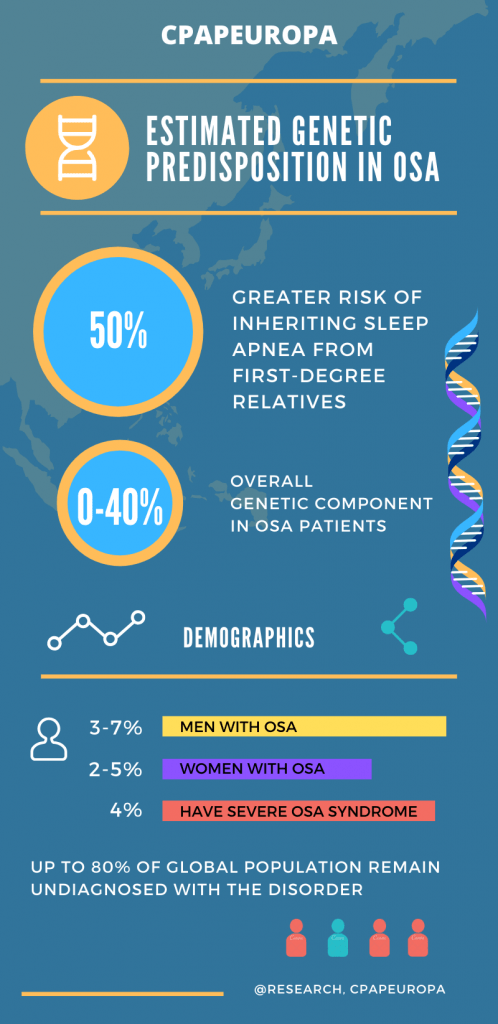
Obstructive sleep apnea (OSA) is a common sleep disorder that occurs when the muscles in the back of your throat fail to keep your airway open, despite the effort to breathe. This leads to periods of time where you stop breathing, or your breathing is significantly diminished, known as apneas or hypopneas. These episodes can last for a few seconds to minutes, and can occur many times during the night.
The most common symptoms of OSA include loud snoring, frequent pauses in breathing during sleep, choking or gasping for air during the night, and feeling excessively tired during the day. However, some people with OSA may not be aware that they have the disorder and are often only diagnosed after a partner notices the symptoms.
OSA is caused by the collapse of the airway during sleep, which can be due to various factors such as obesity, a thick neck circumference, a small jaw and airway or large tonsils and adenoids. OSA can also be caused by structural issues such as a deviated septum, or by neurological conditions such as muscle weakness in the throat. People with OSA may also be more likely to have certain medical conditions such as hypertension, diabetes, and heart disease.
Diagnosis of OSA is usually done through a sleep study, usually a polysomnography test, which is done in a sleep center and records several different measurements such as brain activity, eye movement, muscle activity, and air flow to help evaluate the quality of sleep and confirm the presence of OSA or other sleep disorder.
Treatment for OSA typically involves using a CPAP machine which provides a constant stream of air to help keep the airway open during sleep. Other treatments include lifestyle changes such as weight loss, positional therapy (to avoid sleeping on the back) and in certain cases, surgery can be considered.
It is important to note that OSA is a serious condition that can have significant impacts on quality of life and can have serious consequences on your overall health if left untreated. It is important to consult with a healthcare provider if you suspect that you have OSA.































 WE SHIP CPAP MACHINES WITH EXPRESS 1-DAY DELIVERY (PLEASE MAKE SURE TO SELECT THE 1-DAY DELIVERY OPTION UPON CHEKOUT) TO THE FOLLOWING CANTONS OF SWITZERLAND:
WE SHIP CPAP MACHINES WITH EXPRESS 1-DAY DELIVERY (PLEASE MAKE SURE TO SELECT THE 1-DAY DELIVERY OPTION UPON CHEKOUT) TO THE FOLLOWING CANTONS OF SWITZERLAND: